I know. You have been hearing about Behavioral & Mental Health (BMH) a lot lately. But, there are some new insights regarding the design of healthcare environments that have come to light that I wanted to make sure you knew about. Besides, it’s Mental Health Awareness month.
Designing for Dignity in Behavioral & Mental Health Environments

Mental Health Awareness Month was started in the United States in 1949 by the Mental Health America organization. During the month of May, Mental Health America, its affiliates, and other organizations interested in mental health conduct several activities which are based on a different theme each year. This year’s theme is centered on raising awareness of the brain-body connection through #4mind4body challenges.
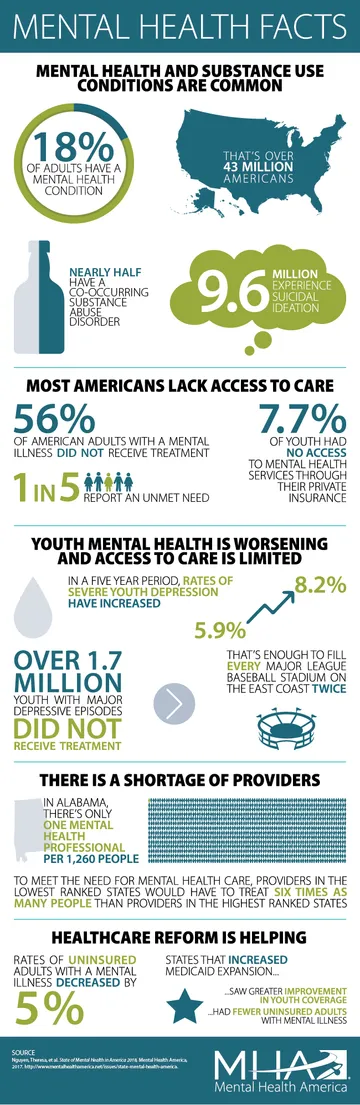
The Stats
- One out of every five adults experience one or more BMH conditions
- 56% of U.S. adults with a mental illness go without treatment
- 80% of adolescents with depression go without treatment (Mental Health America, 2016)
- Access to BMH care is so poor that adults with severe mental illness are 3X more likely to be found in jail or prison than in a psychiatric hospital bed
- Although the perception of patients with behavioral mental health comorbidities is perceived as small, between 25-45% of patients admitted to the hospital for medical care have one or more BMH issues
What have behavioral mental health facilities looked like in the past? Behavioral health environments historically provided treatment in an institution-like setting, not unlike the one depicted in the film Girl, Interrupted. Contemporary design solutions, while still focused on the important aspects of safety and patient protection in private patient environments, recognize that this does not provide an adequately safe environment for these patients. Recent Joint Commission standard changes require incorporating safety measures throughout a BMH facility, clarifying that ligature points and other “self-harm environmental risks” must be identified and removed from all areas of the facility unless they are necessary for the direct treatment of the patient. Safe design is now required throughout the BMH facility, not just in patient-specific areas.
Can you give me an example of how Kahler Slater designs for safety throughout a facility? As noted in the statistics above, many patients with BMH issues begin their visit to a hospital at the Emergency Department. One recent example where Kahler Slater incorporated Evidence Based BMH design is at Froedtert Health’s Community Memorial Hospital in Menomonee Falls, Wisconsin. After analyzing and updating the campus master plan, which identified the need for a new 13,541 square foot Emergency Department (ED), it was important that the ED BMH rooms be flexible for use by the general population as well. The design of the rooms follows a clinical standard established throughout the ED, with additional features to support behavioral health patients such as:
- Anti-ligature door and cabinet hardware
- Power outlets on dedicated GFCI circuits with controls for emergency shut-down by staff
- Hand washing sink with protective pipe covering and anti-ligature controls
- Coiling, overhead door used to isolate the headwall during patient behavioral episodes
- Ligature-resistant, impact-resistant television enclosures
- Impact-resistant gypsum board walls and ceilings
- Tamper-resistant lights and sprinklers
In the overall design of BMH treatment facilities/units, emerging evidence shows the following design features–in addition to designing for safety–are also important (Karlin & Zeiss, 2006; Shepley et al., Shepley & Pasha, 2013)
- A homelike, deinstitutionalized environment that supports patient autonomy and control over their own environment
- A well-maintained and well-organized environment
- Noise control
- Support for privacy
- Access to daylight and views of nature
- Physical access to the outdoors
- Support for feelings of personal safety/security
- Support for social interaction
- Positive distractions
What about an example which incorporates design features that are important specifically for BMH treatment facilities?
Look no further than St. Thomas, Ontario, Canada. St. Thomas Elgin General Hospital (STEGH) is a compassionate organization that values patient-centered care and a healing environment with a goal of delivering an excellent patient care experience. Kahler Slater was the lead for the hospital planning and interior architectural design, in partnership with the Toronto architectural firm Montgomery Sisam for this project. The recently completed project encompasses an 80,000 square foot addition, including a 15-bed acute mental health inpatient unit plus associated mental health ambulatory care facilities, a new emergency department, new surgical and procedural rooms, a day surgery program, and a new sterile processing department.
The new Mental Health program includes:
- Socialization spaces, including a patient lounge and dining area
- A group therapy area and a gym
- An accessible open-air terrace planned for outdoor activities
- A multi-purpose activity room
- Private consultation rooms
- A quiet visiting lounge providing patients with as many options for interaction and respite as their individual care plans allow
Bring it all together. Since those with BMH conditions are more likely than the general population to require medical care, the Center for Health Design (CHD) encourages architects and designers to take a universal approach, arguing that all areas of health facilities ought to be considered for design with BMH in mind. As 1 of 8 EDAC Champion firms in the United States, Kahler Slater is passionate about creating healthcare environments that emphasize all aspects of health and wellness for patients, staff and visitors and works to incorporate the aspects Evidence Based Design in every healthcare project.

